
Australia’s mental-health system is leaving many people to find meaningful support only once they qualify for the NDIS. The ABC reports that psychiatrists describe the scheme as an “ambulance at the bottom of the cliff” and argue that stronger early intervention could prevent disability for some and reduce long-term pressure on the system.
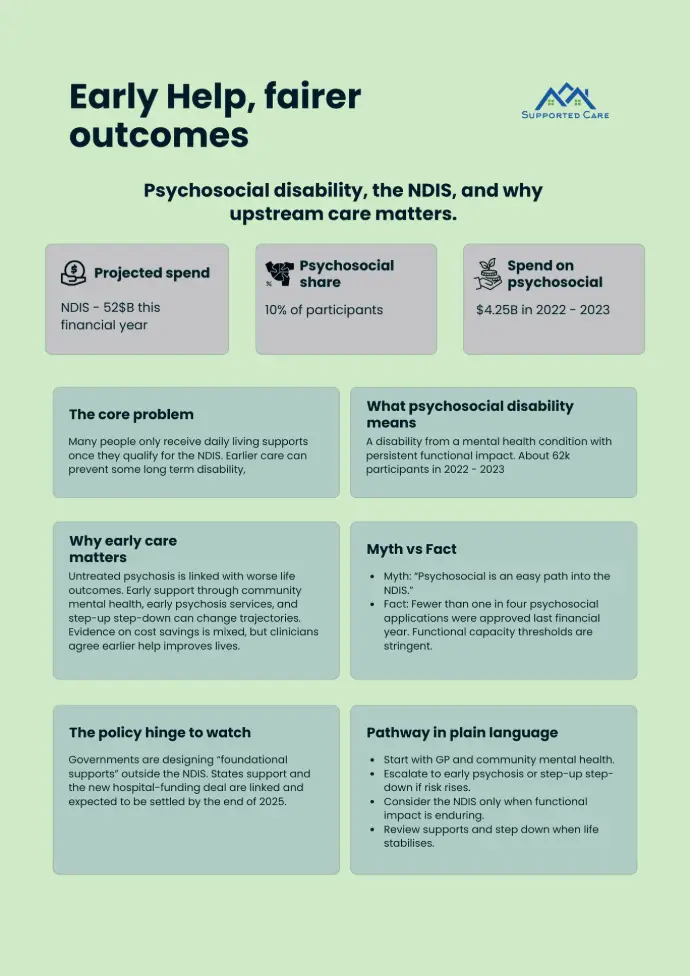
The article notes the financial context that is shaping reform. The NDIS is forecast to cost about $52 billion this financial year, while the Commonwealth seeks to curb growth and shift some psychosocial supports into a new category of “foundational supports”, which depends on a broader state–federal hospital funding deal expected to be settled by year-end.
Psychosocial disability refers to disability that arises from mental-health conditions such as schizophrenia and is the fourth-largest primary disability group in the scheme. In 2022–23 there were about 62,000 participants with a primary psychosocial disability, representing roughly one in ten NDIS participants.

Funding for this cohort is significant. In the year to 30 June 2023, the NDIS paid about $4.25 billion for supports to participants with a psychosocial disability, underscoring why governments and clinicians are debating how much help should be provided earlier in community and hospital settings.
Clinicians quoted by the ABC argue that care is often arriving too late. Early psychosis services and timely hospital care can change life trajectories, whereas untreated psychosis increases the risk of homelessness, justice involvement, and entrenched disability. Others in the sector caution that evidence for cost savings is mixed, while still agreeing that earlier help improves people’s lives.
Advocates also push back against the idea that the NDIS is an easy path. According to the ABC’s reporting, fewer than one in four psychosocial applications were approved in the last financial year, reflecting stringent functional-capacity thresholds and the role that NDIS supports play in daily living once disability is established.
The policy hinge is “foundational supports”, a proposed layer of non-NDIS services jointly designed and funded by the Commonwealth and the states. National Cabinet endorsed the concept in December 2023, and recent communiqués confirm governments are still negotiating scope, timing, and funding. For providers and referrers, this means pathways may soon place more emphasis on community-based psychosocial help before disability becomes permanent.
For families, referrers, and frontline workers, the practical takeaway is simple. Start early with community mental-health supports where available, escalate to specialist early-psychosis or step-up step-down services when risk rises, and consider the NDIS only when functional impact is enduring. This aligns with the ABC’s lived-experience vignette and the clinicians it quotes, while acknowledging that many people will still need disability-level supports to live well.
Key figures at a glance
- NDIS annual cost context sits around the low to mid 50 billions depending on measure and year.
- About one in ten NDIS participants have a psychosocial primary disability. Count about 62,000 as of 30 June 2023.
- Supports to this group totalled about 4.25 billion dollars in 2022 to 2023. Average about 71.6 thousand dollars per participant.
Pathway in plain language
- Start with GP and community mental health.
- Escalate to early psychosis or step up step down services if risk increases.
- Consider NDIS access only if daily function is significantly and persistently affected.
- Review supports and step down when life stabilises while strengthening community links.
Infographic
Psychosocial disability is the ongoing functional impact of a mental health condition on daily life. A person can have a diagnosis without having a psychosocial disability if function is not persistently impaired. As at 30 June 2023 there were about 62,000 participants with a psychosocial primary disability.
Clinicians argue that earlier care improves life outcomes and can reduce the likelihood that disability becomes entrenched. Current practice often responds at crisis points rather than supporting people earlier in their journey.
No. ABC reporting cites lower eligibility rates for psychosocial applicants than the scheme average and highlights stringent functional capacity thresholds.
Foundational supports are services outside the NDIS that governments plan to design and fund jointly so people can access help earlier without needing disability access. National Cabinet endorsed this direction in December 2023 and related work continues through intergovernmental processes and hospital funding talks.
The Australian Institute of Health and Welfare publishes detailed data on psychosocial participation and payments, including the 4.25 billion dollars in supports paid in 2022 to 2023 and the average payment per participant.
Note
This article is general information. It does not replace medical advice. If you are worried about someone’s safety call 000.
Contact us
If you are a family, referrer, or provider and want help navigating options, reach out to our team. We can point you to local community services and discuss next steps.
Ref:
1. Fewer Aussies would need NDIS if government boosted mental health support, expert says - ABC News
2. Mental health services - Mental health - AIHW
3. https://dataresearch.ndis.gov.au/media/3812/download
4. Meeting of National Cabinet – the Federation working for Australia | Prime Minister of Australia